Hemoglobin Disorders
Hemoglobin disorders, also known as hemoglobinopathies, are a group of inherited blood conditions that affect the amount or quality of hemoglobin in the body:
- Hemoglobin: A protein in red blood cells that carries oxygen around the body
- Sickle cell disease: A group of disorders that cause the production of hemoglobin with an abnormal structure and quality
- Thalassaemias: A group of disorders that cause insufficient production of hemoglobin
Hemoglobin disorders are the most common genetic conditions in humans, affecting around 5–7% of the world’s population. However, most carriers lead healthy lives and only develop the disease if they inherit the trait gene from both parents.
Some hemoglobin disorders are severe and require treatment, while others may not cause any symptoms. For example, hemoglobin C disease is an inherited disorder that causes mild anemia, but usually doesn’t cause any problems.
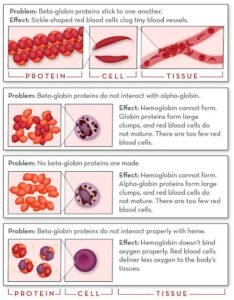
Hemoglobin plays a vital role in the circulatory system, binding to oxygen in the lungs and facilitating its delivery to tissues and organs. When hemoglobin is altered due to genetic mutations, the efficiency of this oxygen transport can be severely diminished, leading to hypoxia and a range of associated health complications. The underlying mechanisms of hemoglobin disorders typically involve mutations in the genes responsible for hemoglobin synthesis, leading to either the production of an abnormal hemoglobin variant or an inadequate quantity of healthy hemoglobin.
Genetic factors are at the heart of hemoglobinopathies. These disorders are generally inherited in an autosomal recessive manner, requiring individuals to receive one copy of the mutated gene from each parent. In certain scenarios, individuals may inherit only one abnormal gene, resulting in a carrier state that often goes unnoticed yet may confer some protective effects against malaria. Nevertheless, carriers can pass on the trait to their offspring, which can lead to the emergence of hemoglobin disorders in future generations.
The ramifications of hemoglobin disorders extend beyond individual health, influencing family dynamics and community health. Early diagnosis and appropriate management are essential to mitigate complications, making awareness of these conditions critical for caregivers, patients, and healthcare professionals alike.
Causes of Hemoglobin Problems
Hemoglobin disorders can arise from a variety of causes that can be broadly categorized into inherited and acquired conditions. Inherited hemoglobin disorders are primarily genetic and are transmitted from one generation to the next. Sickle cell disease, for instance, is a prominent inherited condition characterized by abnormal hemoglobin that leads to distorted, sickle-shaped red blood cells. This shape causes blockages in blood vessels, leading to severe pain and organ damage. Similarly, thalassemia is another genetic disorder that affects hemoglobin production, resulting in anemia and other serious health complications.
Acquired hemoglobin disorders, on the other hand, are not inherited but arise due to external factors impacting the body. Nutritional deficiencies, such as iron deficiency anemia, demonstrate how lacking essential nutrients can lead to decreased hemoglobin levels. Iron, vitamin B12, and folate play crucial roles in red blood cell production, and their deficiency can culminate in diminished hemoglobin concentration, resulting in fatigue and weakness.
Chronic diseases like kidney disease, cancer, and autoimmune disorders can also affect hemoglobin levels. For instance, chronic kidney disease can lead to decreased production of erythropoietin, a hormone essential for red blood cell production, ultimately resulting in anemia. Additionally, environmental factors such as exposure to certain chemicals and pollutants can disrupt normal hemoglobin synthesis. Lifestyle factors, including smoking and excessive alcohol consumption, can further exacerbate these issues by impacting the body’s ability to utilize iron and produce healthy red blood cells.
Understanding the myriad causes of hemoglobin problems is crucial for proper diagnosis and management, underscoring the importance of ongoing research and awareness regarding genetic predispositions and other influencers in this complex area of health.
Pre-Birth Care: Preventing Hemoglobin Disorders
Addressing hemoglobin disorders begins long before an infant’s birth, highlighting the importance of pre-natal care for future mothers. Ensuring optimal maternal health is a critical strategy that can help prevent conditions such as sickle cell disease and thalassemia. One fundamental aspect of pre-natal care is the implementation of genetic screening. This process allows expecting parents to assess their risk of passing on hereditary hemoglobin disorders. Couples with a family history of these conditions are especially encouraged to seek genetic counseling, which can provide valuable information on available tests and the implications of results.
In addition to genetic screening, maintaining a healthy diet plays a vital role in nurturing maternal health. Nutrition is paramount, as certain dietary supplements can influence the risk of hemoglobin disorders. A crucial element in this regard is folic acid; studies demonstrate that adequate levels of folic acid intake can reduce the risk of neural tube defects and may also mitigate the risk of other complications related to hemoglobin. Healthcare providers typically recommend a daily intake of 400 micrograms of folic acid for women planning to conceive.
Iron, another essential nutrient, supports the development of the fetus and helps prevent anemia in mothers, which can complicate pregnancy and affect hemoglobin levels. It is advisable for women to incorporate iron-rich foods, such as lean meats, beans, and fortified cereals, into their diet. Alongside a balanced diet, ensuring regular pre-natal visits enables healthcare providers to monitor a mother’s health and hemoglobin levels, adjusting dietary or supplemental needs as necessary. By taking these proactive steps and focusing on maternal health strategies, prospective parents can significantly reduce the risk of hemoglobin disorders in their children, offering a healthier start to life.
Post-Birth Care: Monitoring and Managing Hemoglobin Levels
The postnatal period is critical for infants as their bodies transition from the womb to independent living. One major aspect of this transition is the careful monitoring of hemoglobin levels to identify and manage any potential hemoglobin disorders. It is essential for caregivers to recognize the significance of regular screenings to ensure early detection and intervention.
Initially, newborns should undergo a blood test, typically within the first week of life, to assess hemoglobin levels. This initial screening helps identify conditions such as anemia or other hemoglobin-related disorders. Parents should be informed about the recommended schedule for follow-up tests, which may vary based on the infant’s health and family history of hemoglobin disorders. Consistent monitoring is crucial, as undiagnosed conditions can lead to serious health complications if left untreated.
Caregivers should also be educated on the signs that may indicate potential hemoglobin disorders. Common symptoms can include unusual pallor, fatigue, and irritability. Additionally, infants might exhibit breathing difficulties or poor feeding habits. It is vital for parents to remain vigilant and report any concerning changes to their healthcare provider promptly. Early recognition of these signs can facilitate timely intervention, improving the likelihood of positive health outcomes.
Providing proper nutrition is another fundamental aspect of managing hemoglobin levels in infants. Exclusive breastfeeding is often recommended for the first six months, as it provides essential nutrients that support healthy hemoglobin production. In cases where supplementation is necessary, parents should consult with their healthcare provider to determine the best approach based on the infant’s specific needs.
In conclusion, proactive post-birth care, involving regular screenings and attentive monitoring of hemoglobin levels, is essential to ensure a healthy start for infants. By being informed and responsive, caregivers can play a pivotal role in managing their child’s health and well-being effectively.
Thyroid Health: Natural Balance and Recovery
Medication for Hemoglobin Disorders in Children
Managing hemoglobin disorders in children often involves a range of medications designed to alleviate symptoms and improve overall health. One of the most common treatments prescribed is iron supplementation. Iron is critical for the production of hemoglobin, and children with certain hemoglobin disorders, such as thalassemia, may require additional iron to support their hemoglobin levels. Physicians typically determine the need for iron supplements through regular blood tests and health assessments, as excessive iron can lead to complications. Therefore, healthcare providers usually monitor iron levels to customize treatment appropriately.
Another significant medication used in the management of hemoglobin disorders is hydroxyurea. This drug primarily assists patients with sickle cell disease, aiming to reduce the frequency of pain crises and the need for blood transfusions. Hydroxyurea works by increasing fetal hemoglobin levels, which helps to inhibit the sickling of red blood cells. It is typically taken as a daily oral medication, and while it can be effective, it may also present potential side effects, such as changes in blood counts and risks of infections. Physicians must weigh the benefits against risks and may adjust the dosage based on individual patient response.
Blood transfusions are another crucial component of medication for children with hemoglobin disorders. These procedures are often necessary for those with severe anemia or frequent pain crises. Blood transfusions can provide immediate relief by increasing the number of healthy red blood cells in circulation. However, they come with some risks, including allergic reactions and iron overload. Regular monitoring after transfusions is vital to ensure the child’s safety and to manage any side effects that may arise.
In conclusion, the management of hemoglobin disorders in children involves a comprehensive approach through medications such as iron supplements, hydroxyurea, and blood transfusions. Each treatment has its advantages and potential side effects, necessitating careful oversight by healthcare providers to ensure the best outcomes for young patients.
Natural Remedies and Lifestyle Changes
Managing hemoglobin disorders effectively often requires a multifaceted approach, incorporating not just medical treatments but also holistic remedies and lifestyle adjustments. One of the first steps individuals can consider is making specific dietary changes. A balanced diet rich in iron, folate, and vitamins can play a vital role in supporting hemoglobin production. Foods such as leafy greens, lean meats, beans, and fortified cereals should be emphasized. Additionally, vitamin C-rich foods, like oranges and strawberries, can enhance iron absorption, making it crucial to pair such foods together for optimal nutritional benefits.
Herbal supplements have gained attention as complementary treatments for managing hemoglobin disorders. For instance, herbs such as nettle and dandelion are often cited for their potential blood-building properties. These herbs can be consumed in teas or capsules, but it is essential to consult with a healthcare professional before starting any supplement regimen, as interactions with prescribed medications may occur.
Incorporating physical activity into one’s routine can greatly influence overall well-being and assist in managing symptoms associated with hemoglobin disorders. Engaging in moderate exercise, such as walking or yoga, can enhance circulation and energy levels. Exercise also aids in stress reduction, which is another significant aspect of care. Stress management techniques, such as mindfulness meditation or deep-breathing exercises, can contribute to controlling anxiety and fostering emotional resilience, ultimately benefiting individuals living with these disorders.
In summary, employing natural remedies and making lifestyle changes, including dietary adjustments, including herbal supplements, regular physical activity, and effective stress management techniques, can yield significant benefits for those affected by hemoglobin disorders. Combining these holistic approaches with conventional medical advice creates a more comprehensive care plan tailored to individual needs.
The Role of Nutrition in Hemoglobin Health
Nutrition plays a pivotal role in maintaining overall health, particularly when it comes to hemoglobin levels. Hemoglobin, the protein in red blood cells responsible for transporting oxygen throughout the body, is influenced by various dietary components. Essential nutrients such as iron, vitamin B12, and folate are crucial for the production and maintenance of healthy hemoglobin levels. An adequate intake of these nutrients can significantly impact individuals suffering from hemoglobin disorders.
Iron is one of the most critical minerals for hemoglobin production. It serves as a central component of hemoglobin, and its deficiency can lead to anemia, characterized by reduced oxygen transport in the blood. Iron can be sourced from two types of food: heme iron, found in animal products such as red meat and poultry, and non-heme iron, found in plant-based foods like legumes, nuts, and green leafy vegetables. For optimal absorption, it is beneficial to pair iron-rich foods with vitamin C sources, such as citrus fruits or bell peppers.
Vitamin B12 is another vital nutrient that supports hemoglobin synthesis. It primarily exists in animal-derived foods such as fish, meat, eggs, and dairy products. Individuals following a vegetarian or vegan diet may be particularly susceptible to B12 deficiency and should consider fortified foods or supplements. Likewise, folate, also known as vitamin B9, is necessary for DNA synthesis and red blood cell formation. Folate can be found in abundance in dark leafy greens, beans, peas, and fortified cereals.
Creating a balanced diet that incorporates these essential nutrients can help support individuals with hemoglobin issues. Ensuring a diverse array of food choices not only aids in maintaining adequate hemoglobin levels but also contributes to overall well-being. It is advisable to consult with a healthcare professional or a registered dietitian to tailor dietary approaches that meet individual nutritional needs, particularly for those managing specific hemoglobin disorders.
Understanding Accountant Services in the UK: A Comprehensive Guide
hemoglobin disorder and treatment: Strategies for Families
Families affected by hemoglobin disorders often face unique challenges that can impact their emotional well-being and daily lives. Employing effective coping strategies is essential to help families navigate these complexities successfully. One of the most crucial aspects is providing emotional support to each family member. Open communication is key; discussing feelings, fears, and experiences can foster a supportive environment. Families can benefit from support groups, where they can share experiences and connect with others facing similar challenges, thereby reducing feelings of isolation.
Educational resources play a significant role in empowering families. Gaining knowledge about hemoglobin disorders—including symptoms, treatment options, and potential complications—can help families make informed decisions regarding care. Local hospitals, universities, and online platforms often provide valuable information that can be accessed easily. Moreover, workshops and seminars on hemoglobin disorders can equip caregivers with the tools necessary for effective management and support. This education can lead to a better understanding of the specific needs of their loved ones, promoting proactive care.
Community involvement is another critical coping strategy. By engaging with local organizations that focus on hemoglobin disorders, families can find additional resources and support networks. Participating in fundraising events or awareness campaigns can foster a sense of purpose and solidarity while raising important funds for research and support initiatives. Furthermore, involving friends and extended family in the caregiving process can alleviate stress and provide additional emotional support, creating a more robust support system for those affected. By integrating these coping strategies, families can navigate the complexities of hemoglobin disorders more effectively, enhancing their overall well-being and resilience.
Conclusion and Resources
Hemoglobin disorders are a complex group of conditions that arise due to abnormalities in the hemoglobin molecule, fundamentally affecting oxygen transport within the body. Throughout this blog, we have explored the various causes of these disorders, including genetic mutations that lead to conditions such as sickle cell disease and thalassemia. Understanding these underlying mechanisms is crucial for proper diagnosis and treatment strategies, providing a solid foundation for families impacted by these diseases.
Moreover, the care and management of hemoglobin disorders require comprehensive approaches that incorporate medical treatment, ongoing monitoring, and psychological support. Caregivers and families must be educated about the specific disorder affecting their loved one to better navigate the healthcare system and make informed decisions regarding treatments and lifestyle adaptations. The importance of a supportive network, including healthcare professionals, support groups, and community resources, cannot be overstated in ensuring holistic support for those affected.
For families seeking further information on hemoglobin disorders, numerous resources are available. Organizations such as the Sickle Cell Disease Association of America and Thalassemia International Federation provide educational materials, support networks, and advocacy services. Additionally, numerous academic publications and journals discuss the latest research findings and treatment options, making them excellent references for families wanting to delve deeper into the subject. Consulting with a knowledgeable hematologist can also provide personalized guidance tailored to individual circumstances.
By prioritizing education and fostering community support, families dealing with hemoglobin disorders can cultivate resilience and hope. They are encouraged to reach out for professional guidance and engage with local support networks, ensuring they are well-equipped to manage the challenges associated with these conditions. Ultimately, understanding hemoglobin disorders empowers families to navigate their journeys confidently, knowing they are not alone on this path.